Researchers develop a faster, better way to disinfect N95 masks for reuse
A team of University of Chicago researchers has developed a better, faster way to decontaminate N95 masks using ultraviolet light—potentially saving thousands of the sought-after masks during the COVID-19 pandemic.
The system is currently in use at the hospital at the University of Chicago, and the team is working with the Polsky Center for Entrepreneurship and Innovation to certify and scale it up for wider use.
Ultraviolet C, a wavelength of light with the ability to kill germs, has emerged as the preferred solution for disinfecting personal protective equipment. But even though it is easy to deploy and widely applicable, the method is not without its drawbacks; as with any light, UV systems can cast shadows, leaving parts of surfaces in the dark.
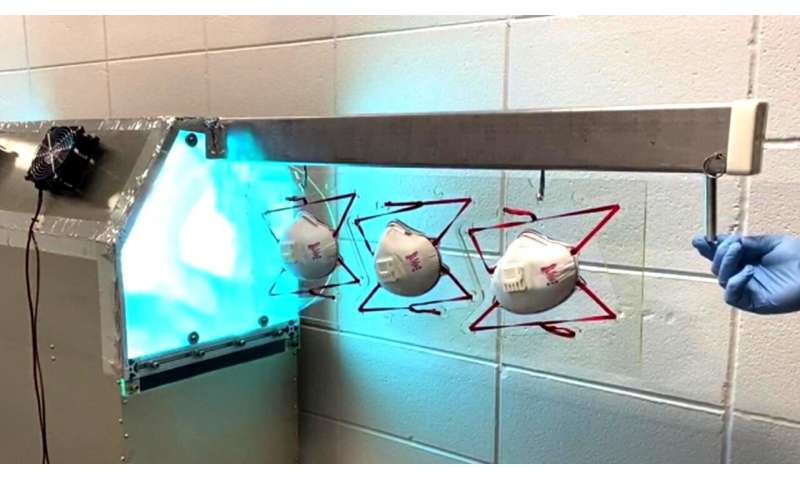
To address this issue, Peter Eng, an experimental physicist and research professor at UChicago, designed and fabricated an N95 respirator decontamination cabinet, which features a UV lamp arrangement that eliminates shadowing and optimizes the dose to all surfaces of the mask.
The current setup can fully disinfect 180 masks per hour, and the inventors estimate a scaled-up, automated version could process up to 1,440 masks per hour—or more than 34,000 per day.
A breakthrough after a restless night
Eng, who uses an ultraviolet curing system in his lab at the Center for Advanced Radiation Sources based at Argonne National Laboratory, came up with the idea for the decontamination cabinet in mid-March, during the first days of Chicago’s shelter-in-place order.
Unable to sleep one night, he got out of bed and began researching different decontamination techniques. By morning, he had discovered a large body of published work that indicated UV irradiation was effective in rendering viruses inactive and began placing calls to various researchers. Based on this information, he made a few preliminary calculations and produced a 3-D Solidworks model and a list of components for a dedicated N95 mask disinfection device.
“Being a scientist working in the research world—specifically in designing equipment that we use for doing experiments—I’m used to contacting authors and companies, so I just started reading papers and developing a database,” said Eng.
The next day, Asst. Prof. Naoum Issa, head of epilepsy research at the University of Chicago Medicine, put Eng in contact with Jon Brickman, the hospital’s executive director of perioperative and procedural service. Brickman, whose job includes preserving PPE, helped Eng define the requirements for a system that would meet the needs of the medical center. Issa also provided his clinical input on methods and needs for disinfection protocols.
“In talking with Jon, I discovered that he had an urgent need to start a disinfection process using existing high-powered UV disinfection units that the hospital already owned,” Eng said.
Eng began looking into the details of these units and a way to temporarily repurpose the hospital’s equipment to disinfect an array of masks, instead of the operating and patient care rooms for which the units were designed.
Brickman described Eng as the catalyst for moving from “we can do this with the units we have” to “we can do this better.”
“Senior leadership recognized early on that a national shortage of N95 respirators would require us to act swiftly to preserve and extend our inventory,” said Brickman. “Based on the literature at the time and access to readily available commercial UV disinfection units made ultraviolet germicidal irradiation an attractive option for our facility.”
With copper piping and a blowtorch in hand, Eng spent the weekend working with his friend, artist and carpenter Steve Badgett, soldering a frame structure to hold the masks. A few days later, Eng and Badgett delivered five rolling frames to Brickman, along with a detailed room map that marked out the placement of the lamp towers around the N95 mask frame. Then they ran extensive tests to make sure the arrays were in fact thoroughly disinfecting the masks.
UChicago Medicine has been using the system to disinfect masks since the beginning of April. Over the course of the pandemic, reprocessing could save the academic health system thousands of the hard-to-come-by masks.
Even faster methods
Once the temporary hospital system was up and running, Eng turned his focus to developing a new system from scratch that could thoroughly decontaminate masks at a much higher rate.
A week after assembling his team, Eng built and tested the prototype—a sort of cabinet. To disinfect masks, you simply load the masks in racks, a few at a time, and wait as a bath of light moves through.
“By optimizing the light array inside the box, you evenly illuminate all the surfaces and minimize the amount of time it has to be in there,” said Eng—noting that it also is vital that no one surface of the mask is subject to much more light than any other. This is important because a mask can only receive so much irradiation before it starts to break down and has to be discarded.
“It’s not simply the number of times it goes through the system; it’s the sum total of irradiation,” Eng explained. “By homogenizing that pattern, it maximizes the number of disinfection cycles.”
The hospital has begun using the cabinet system to disinfect more masks. A second version is also in the works, and Eng is actively working with the Polsky Center for Entrepreneurship and Innovation to talk with product design companies. Next steps include evaluating the design and completing any necessary changes in order to produce a set of drawings that could be used by a manufacturer. In the future, the system could benefit other industries as well.
“It’s a process that I can easily imagine in a factory,” said Eng, who used to work on a packaging line at a food supply company. Still, backed with published articles and measurements of the actual system, he said the numbers speak for themselves: “That makes me feel like I can sleep. It also lets people make their own decisions—I’m not giving you advice, I’m giving you the source of information.”
Source: Read Full Article


