The ‘Christchurch mutation’: How good can overpower evil in the genetic determination of Alzheimer’s disease
Researchers at Gladstone Institutes have discovered that a rare genetic variant known as the “Christchurch mutation” can block detrimental effects of apolipoprotein E4, the best-established risk factor for the most common form of Alzheimer’s disease.
The apolipoprotein E (APOE) gene has long been known to affect the risk of Alzheimer’s disease through its three main variants: E2 (low risk), E3 (intermediate risk), and E4 (high risk). More recently, a genetic change in this gene, the “Christchurch mutation,” was identified in a woman who did not develop Alzheimer’s disease, even though she had inherited another gene that causes a very rare but highly aggressive form of the disease, raising the possibility that the Christchurch mutation may protect against Alzheimer’s disease.
Now, researchers at Gladstone Institutes investigated whether the Christchurch mutation can also protect against the detrimental effects of APOE4, which is an important risk factor for the most common form of Alzheimer’s disease. The scientists found that engineering the Christchurch mutation into the APOE4 gene reduces the APOE4-dependent accumulation of the protein tau, neuroinflammation, and neurodegeneration in models of Alzheimer’s disease.
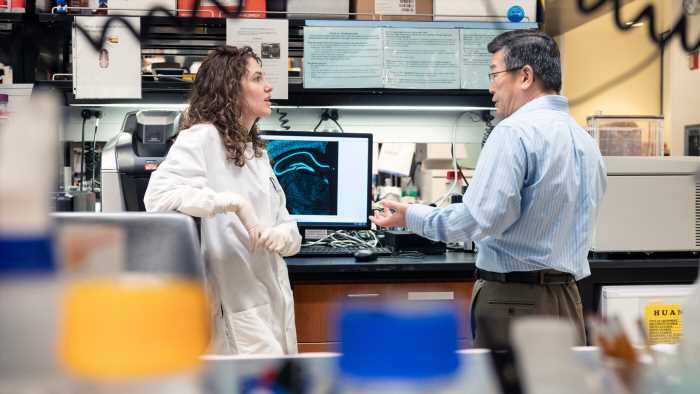
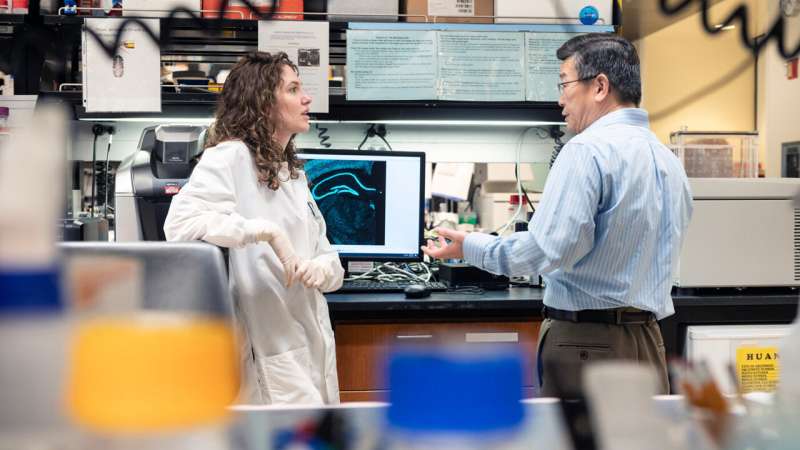
“It’s really exciting that the Christchurch mutation can lead to such broad protection,” says Gladstone Investigator Yadong Huang, MD, Ph.D., senior author of the new study published in Nature Neuroscience. “It opens the door to novel therapeutic interventions that could mimic the beneficial effects of this mutation.”
Complex genetics
In 2019, researchers learned about the woman near Medellin, Colombia, who escaped her family’s fate of early-onset Alzheimer’s disease. She and many of her extended family carried a variant of the PSEN1 gene that causes a rare but very aggressive form of early-onset Alzheimer’s.
She, however, also carried another mutation—a tiny change in the APOE gene known as the Christchurch mutation. The same mutation had been identified decades earlier in a family in Christchurch, New Zealand, and was shown to impact cholesterol levels and heart disease.
“It seemed likely that this woman was protected from early-onset Alzheimer’s disease because of the APOE Christchurch mutation,” says Huang, who is also director of the Center for Translational Advancement at Gladstone, and professor of neurology and pathology at UC San Francisco. “We immediately wondered whether this mutation could also be protective against late-onset Alzheimer’s, which accounts for the vast majority of cases of the disease.”
Huang’s lab had already been studying the impact of APOE4 on brain cells and had developed strains of mice, whose own APOE genes were replaced with human APOE genes, and that also produces the human tau protein, which accumulates in the brain with aging and in Alzheimer’s disease.
Maxine Nelson, Ph.D., a former graduate student in Huang’s lab and lead author of the new paper, and her collaborators further engineered those strains of mice to also have the Christchurch mutation. They also used CRISPR gene editing to alter the APOE4 gene in human induced pluripotent stem cells, which had been generated from an Alzheimer’s disease patient’s blood cells and then developed into mature neurons in a dish.
“It was amazing to be able to bring all these technologies together to answer a question that had significant implications for both research and patients,” says Nelson.
Broad protection
In mice that carried human APOE4 and tau genes but lacked the Christchurch mutation, the researchers saw many of the expected signs of Alzheimer’s disease. The tau protein accumulated in neurons, levels of neuroinflammation increased in the brain, and immune cells known as disease-associated microglia became more prevalent.
Remarkably, introducing the Christchurch mutation into these mouse models prevented or markedly reduced these abnormalities.
By comparing human neurons that produced APOE4 with or without the Christchurch mutation in cell culture, the researchers were able to identify molecular mechanisms that could contribute to the beneficial effects of the mutation in the brain.
These mechanisms relate to the transfer of tau from the outside to the inside of neurons, which might contribute to neuronal impairments in Alzheimer’s disease. This transfer, or uptake, of tau is mediated by cell surface molecules called heparan sulfate proteoglycans (HSPGs) and, as it turns out, is strongly affected by APOE and the Christchurch mutation.
That APOE interacts with HSPGs was demonstrated 30 years ago by Gladstone Investigator Robert Mahley, MD, Ph.D., who is also a co-author of the recently published study.
In the new study, the scientists found that the Christchurch mutation strongly reduces the ability of APOE4 to bind HSPGs and that this effect leads to a marked reduction in neuronal tau uptake.
“The results suggest that blocking the interaction of APOE4 with HSPGs could help treat or prevent Alzheimer’s disease in people with the APOE4 gene,” Huang says. “This might be accomplished with small molecule drugs, monoclonal antibodies, or gene therapy. However, more work is needed before such treatments can be developed and tested.”
The paper, “The APOE-R136S mutation protects against APOE4-driven Tau pathology, neurodegeneration and neuroinflammation,” was published in the journal Nature Neuroscience.
More information:
The APOE-R136S mutation protects against APOE4-driven Tau pathology, neurodegeneration and neuroinflammation, Nature Neuroscience (2023). DOI: 10.1038/s41593-023-01480-8
Journal information:
Nature Neuroscience
Source: Read Full Article