Study suggests T-cells don't determine survival in severe COVID-19
The coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causes mild to moderate illness in the general population. Some people, however, may experience severe symptoms, which can be potentially fatal.
Severe COVID-19 has been tied to T cell lymphopenia, but no causal effect of T cell deficiency on disease severity has been established.
Researchers at the Laboratory of Persistent Viral Diseases, Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, National Institutes of Health found that T cell-depleted groups of rhesus macaques developed virus-neutralizing antibody responses and also class-switched to immunoglobulin G (IgG).
In the study, which appeared on the pre-print server medRxiv*, the team found that when the monkeys were reinfected, the T cell-depleted animals showed anamnestic immune responses, the enhanced reaction of the body's immune system to an antigen that is related to an antigen previously encountered.
This is characterized by the rapid induction of high-titer virus-neutralizing antibodies, faster control of viral loads, and decreased symptoms or clinical signs.
Study background
Previous studies suggest that T cells or T lymphocytes play imperative roles in COVID-19. For instance, it has been shown that COVID-19 convalescent patients, or those who recovered from the illness, possess both CD4+ and CD8+ T cells responsive to SARS-CoV-2 antigens.
Also, severe COVID-19 has been linked to lymphopenia, the reduced amount of white blood cells in the blood. During an infection, like COVID-19, white blood cells attack, bind to, and help stimulate the production and secretion of chemicals to fight the virus. There is also the loss of both CD4+ and CD8+ T cells.
However, it is still unclear whether lymphopenia contributes to severe COVID-19 or an effect of the disease.
The study
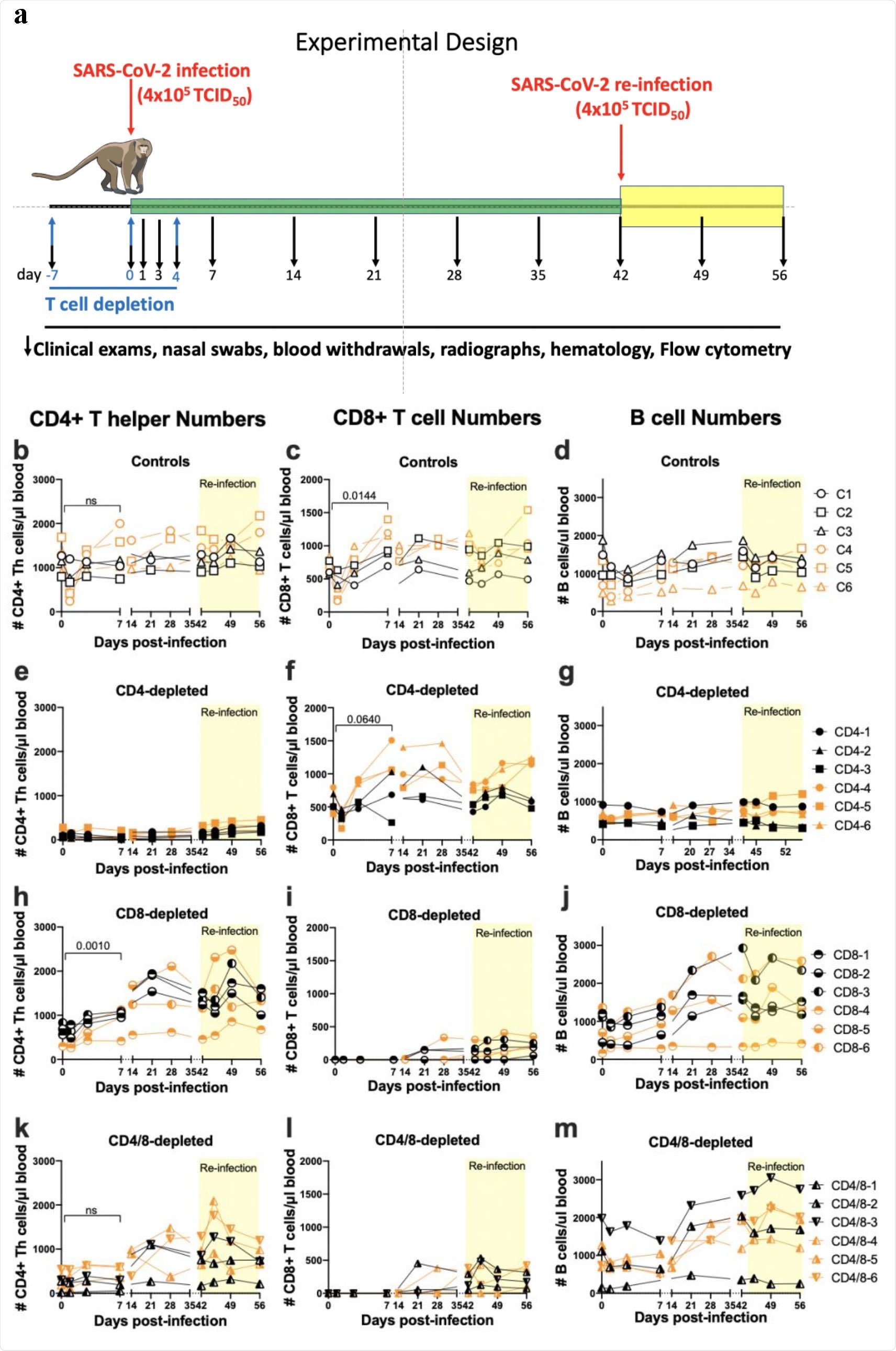
To provide definitive proof of T cells' importance in recovery from infection and the development of anamnestic responses, the researchers studied adult rhesus macaques depleted of either CD4+, CD8+, or both T cells subsets before infection with SARS-CoV-2.
Like most adult humans, rhesus macaques only become mildly or moderately affected. They do not usually develop acute respiratory distress syndrome (ARDS), a severe complication of COVID-19.
A better understanding of the immunological mechanisms contributing to the development of resistance in these animals can help future vaccine studies. It can help in the development of new vaccines, therapeutics, and prophylactics.
The researchers focused on T cells' role in resolving acute SARS-CoV-2 infection and developing immunological memory. This provides better protection from potential re-infection in the future.
The researchers inoculated the macaques with the Washington isolate of SARS-CoV-2 and rested for six weeks to arrive at the study findings. From there, the team challenged the animals a second time. They conducted two separate experiments, each with three animals per group for a total of six macaques per group.
The team revealed that CD4+ and CD8+ T cells' depletion only slightly prolonged the monkeys' recovery from their first infection. These cells had little or no impact on the recovery from re-infection. This does not mean that T cells have no role in controlling SARS-CoV-2 infections. However, the roles do not appear as necessary, which means their loss can be compensated by other immune cells.
Further, there is no evidence that T cells play a role in developing the disease in monkeys. The team found that disease severity in monkeys who are T cell replete was similar to the T-cell depleted animals.
The team also showed that old age in humans plays a vital role in vulnerability to severe illness and death from COVID-19. Advanced age is linked to immunosenescence, which makes them easily infected with pathogens. This means that older adults are at a higher risk and are less able than adult monkeys to compensate for immune deficiencies, including SARS-CoV-2-induced lymphopenia.
When it comes to rhesus macaques, older monkeys develop lower antibody responses to SARS-CoV-2 infections. This means that different results will be obtained using older animals.
"That said, our results from adult macaques with profound depletion of either CD4 + or CD8+ T cells leads to the conclusion that neither subset played a critical role in their recovery from acute disease or re-infection. On the other hand, anamnestic antibody responses were strongly associated with recovery from a second infection and reduced disease," the team concluded in the study.
The team suggests further studies, particularly among older monkeys, to see if the same results will come out. Furthermore, human studies are also needed.
*Important Notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Hasenkrug, K., Feldmann, F., Myers, L. et al. (2021). Recovery from acute SARS-CoV-2 infection and development of anamnestic immune responses in T cell-depleted rhesus macaques. medRxiv. https://www.biorxiv.org/content/10.1101/2021.04.02.438262v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Acute Respiratory Distress Syndrome, Allergy, Antibodies, Antibody, Antigen, Blood, CD4, Cell, Coro, Coronavirus, Coronavirus Disease COVID-19, Cytometry, Flow Cytometry, Immune System, Immunoglobulin, Infectious Diseases, Laboratory, Lymphocyte, Lymphopenia, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, T-Cell, Therapeutics, Vaccine

Written by
Angela Betsaida B. Laguipo
Angela is a nurse by profession and a writer by heart. She graduated with honors (Cum Laude) for her Bachelor of Nursing degree at the University of Baguio, Philippines. She is currently completing her Master's Degree where she specialized in Maternal and Child Nursing and worked as a clinical instructor and educator in the School of Nursing at the University of Baguio.
Source: Read Full Article


