Pipeline of cell and gene therapies holds promise for repairing the Parkinson’s-damaged brains
After several decades of pre-clinical development, cell- and gene-based therapies for Parkinson’s disease (PD) are now actively being explored. In this special supplement to the Journal of Parkinson’s Disease, “Repairing the Parkinsonian Brain,” experts highlight some of the current strategies being pursued to restore lost function and replace what is lost in the PD brain, with special emphasis on the challenges associated with translating advanced therapeutic approaches into pioneering clinical trials.
“Cell and gene therapy for brain diseases have been long in the making, from the first speculative ideas and the first exploratory trials in the 1980s and 1990s to the major setbacks in the cell and gene therapy fields at the turn of the century, followed by the renewed developments seen during the last decade,” explained Guest Editors Anders Björklund, Ph.D., Bastiaan R. Bloem, MD, Ph.D., Patrik Brundin, MD, Ph.D., and Howard Federoff, MD, Ph.D.
“This revival of the cell and gene therapy field has been driven by the remarkable technical developments that have given us access to increasingly more powerful molecular and genetic tools and techniques. It has opened up far more refined approaches to therapy for neurodegenerative diseases, and PD in particular,” noted co-Guest Editor Patrik Brundin, MD, Ph.D., Parkinson’s Disease Center, Department of Neurodegenerative Science, Van Andel Institute, Grand Rapids, MI, U.S.. “This development has gained new momentum over the last few years through the active involvement of the biotech industry, sometimes in partnership with large pharmaceutical companies.”
Pioneering trials in this field face regulatory and ethical challenges that are radically different from those applied to conventional drug trials. In Part I on the path to clinical trials for advanced therapies, experts review the challenges involved in the design and conduct of the early clinical trials; the different and complementary perspectives on regulatory and safety requirements; and the design and initiation of first-in-man trials. Ethical issues are explored from the investigator’s, scientist’s, ethicist’s, and patient’s perspective. including the patient´s concerns related to participation as a subject in demanding trials that extend over the long-term, where the outcome and risks are uncertain.
The use of advanced therapy medicinal products (ATMPs) including cell and gene treatments, are reviewed both from the investigator’s perspective and the patient’s perspective. Roger A. Barker, MBBS, Ph.D., Department of Clinical Neuroscience, University of Cambridge; and MRC-WT Cambridge Stem Cell Institute, Cambridge, UK, and coauthors point out that investigators taking an ATMP to clinical trials in patients with PD should ask themselves two key questions before embarking on such work: firstly, why are you doing it, and, secondly, do you understand what is needed to conduct a clinical trial with that product. “For ATMPs, there is an enhanced requirement for safety reporting to the regulatory authorities,” noted Dr. Barker. “For example, it is imperative when conducting a trial across countries with different regulatory authorities that there is a central reporting process to capture the safety events from the trial.”
For patients, a reasonable definition of an ideal advanced therapy is one that addresses one or more unmet needs of patients not covered by existing therapies, treatments with a novel mechanism of action, and most importantly, an intervention that has the potential to be disease-modifying, according to two patient advocates/scientists, Soania Mathur, MD, UnshakeableMD, Oshawa, ON, Canada, and Jon Stamford, Ph.D., DSc, neuroscientist and independent Parkinson’s advocate. They review the issues surrounding engaging the patient community in bringing advanced therapies to the clinic, physician-patient communication, and informed consent from the patient perspective.
Participation in clinical trials and clinical use of advanced therapies have their own risk profile above and beyond standard therapeutics as evidenced by past invasive procedures. Dr. Mathur and Dr. Stamford point out that, “It is of utmost importance that clear, evidence-based information about these potential treatments is clearly communicated by those exploring their use to ensure safe and informed participation from the patient community. Patients must be able to weigh the benefits of these treatments, their limitations, and risks in order to truly give informed consent to participate in bringing these treatments to the clinic.”
“The ethical and regulatory issues related to these more advanced treatment modalities are radically different from those involved in standard drug trials in that they must allow for a gradual optimization and perfection of the product, its dosing, and delivery,” noted co-Guest Editor Anders Björklund, Ph.D., Wallenberg Neuroscience Center, Lund University, Sweden. “This requires that implementing novel cell- and gene-based therapies is done in a step-wise, incremental manner, which does not easily fit within the standard Phase I-III design of clinical drug trials.”
The articles in Part II of this supplement highlight research promoting further development of cell and gene therapies.
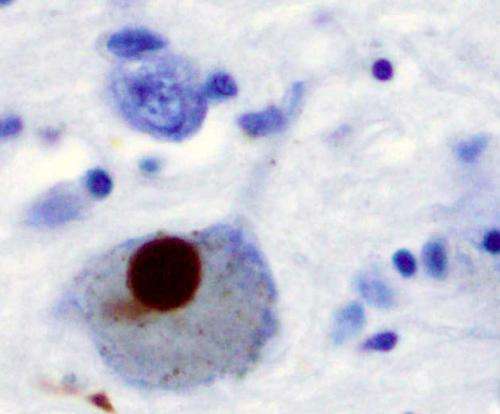
Dr. Björklund and Malin Parmar, Ph.D., Department of Experimental Medical Science, Developmental and Regenerative Neurobiology, Wallenberg. Neuroscience Center, Lund University, Lund, Sweden, note that a limitation of the intrastriatal grafting approach, currently in clinical trial, is that the midbrain dopamine neurons are implanted into the target area and not in the ventral midbrain where they normally reside. This ectopic location of the cells may limit their functionality. They review impressive results with implanting the cells into the substantia nigra in rodent PD models as a way to achieve more complete circuitry repair. “This results in a remarkable degree of circuitry reconstruction that far exceeds what has been possible with ectopic intrastriatal grafts and raises the question whether intranigral transplantation should also be explored in human patients,” they commented.
Many of the potentially causative and risk associated genes for PD are implicated in lysosomal function or lysosomal trafficking, indicating that lysosome dysfunction is a common denominator underlying PD disease pathology. Franz Hefti, Ph.D., CEO, Prevail Therapeutics (wholly-owned subsidiary of Eli Lilly and Company), New York, NY, U.S., and colleagues, review the latest research on one of the lysosomal genes involved, GBA1, which encodes the lysosomal enzyme glucocerebrosidase (GCase) and has the largest impact on PD risk. Studies in mouse models indicate that a vector-based gene therapy designed to deliver a functional GBA1 gene to the brain may slow or stop disease progression.
Source: Read Full Article


