Markers may predict patient response to immune therapy of cancer
For many individuals with different types of cancer, immune checkpoint inhibitors can effectively boost their immune system to fight their disease, but not all patients benefit from these medications. Now a team led by investigators at Massachusetts General Hospital (MGH) and Harvard Medical School (HMS) has developed an approach to help identify potential clinical markers that may indicate which patients will respond to immune checkpoint inhibitors and which should be treated with other strategies. The findings are published in the Proceedings of the National Academy of Sciences.
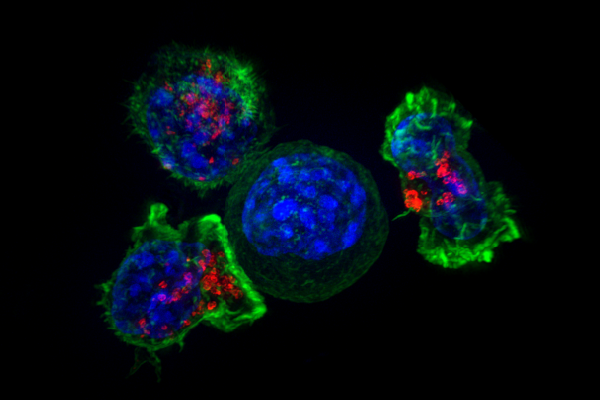
For the study, the scientists developed an approach whereby they implanted breast cancer tumors into mice and then treated the animals with immune checkpoint inhibitors. “We first developed a resection and response bilateral tumor model in which we put one breast tumor in each side of the mouse breast. We then remove one tumor to evaluate the tumor microenvironment and we monitor the response of the other, non-resected, tumor to immune checkpoint blockade, identifying the mouse as a responder or a non-responder,” explained lead author Ivy X. Chen, Ph.D., a former postdoctoral fellow at MGH’s E.L. Steele Laboratories for Tumor Biology. Using this model system, the researchers found that the responding tumors contained higher numbers of cancer-killing “cytotoxic” T immune cells and fewer numbers of certain immune suppressor cells early after the start of treatment.
Gene expression analyses of the cytotoxic T cells within the tumors revealed distinct gene signatures distinguishing responders from non-responders—specifically, the presence of T cell activation signals in responding tumors and T cell exhaustion signals in non-responding tumors. “Importantly, we found that these gene signatures for responder and non-responder tumors significantly correlated with responder and non-responder gene signatures derived from patients with melanoma who were treated with immune checkpoint inhibitors, as well as with overall survival in a group of patients with breast cancer,” said co-senior author Meromit Singer, Ph.D., an Assistant Professor in the Department of Data Science at the Dana-Farber Cancer Institute and the Department of Immunology at Harvard Medical School.
Source: Read Full Article


