Coronavac COVID-19 vaccine safe in children and adolescents and triggers antibodies
Two doses of CoronaVac are safe and provoke a strong antibody response among children and adolescents aged 3-17 years, according to a randomised controlled trial of 550 young people published in The Lancet Infectious Diseases journal.
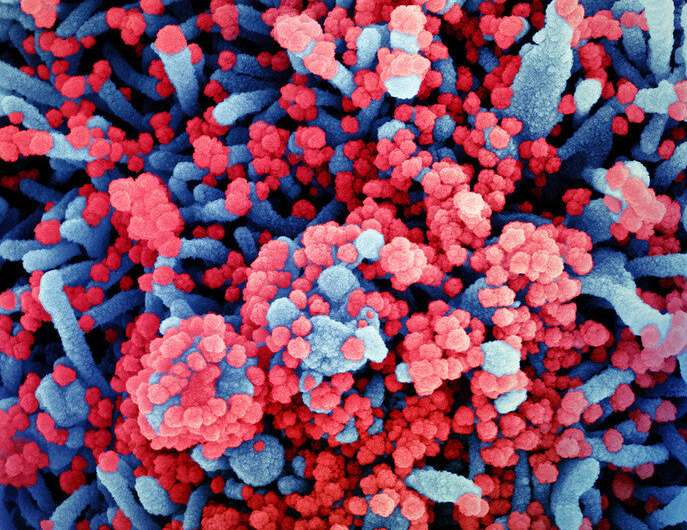
More than 96% of children and adolescents who received two doses of the vaccine—manufactured by Sinovac—developed antibodies against SARS-CoV-2. Most adverse reactions were mild or moderate, with pain at the injection site the most commonly reported symptom.
Qiang Gao, of Sinovac Life Sciences Co, Ltd, China, said: “Children and adolescents with COVID-19 usually have mild or asymptomatic infections compared with adults; however, a small number may still be at risk of severe illness. They can also transmit the virus to others, making it vital to test the safety and effectiveness of COVID-19 vaccines in younger age groups. Our finding that CoronaVac was well tolerated and induced strong immune responses is very encouraging, and suggests that further studies in other regions, involving larger, multi-ethnic populations, could provide valuable data to inform immunisation strategies involving children and adolescents.”
The authors conducted a randomised, double-blind, controlled phase 1/2 clinical trial of CoronaVac in healthy children and adolescents aged 3-17 years in Zanhuang County, China. Between October 31 and December 2, 2020, 72 participants were enrolled in phase 1, with 480 participants enrolled in phase 2 between December 12 and December 30, 2020. The vaccine (either 1.5μg or 3μg per dose) or a control was given by intramuscular injection in two doses, at day 0 and day 28. In studies involving adults aged 18-59 years and people aged 60 years and older, participants received two doses of 1.5μg, 3μg, or 6μg, with 3μg doses suggested for use in further research.
Among the 550 participants who received at least one dose of vaccine or the control, adverse reactions within 28 days occurred in 56 (26%) of 219 participants in the 1.5μg group, 63 (29%) of 217 in the 3μg group, and 27 (24%) of 114 in the control group. Most adverse reactions were mild or moderate, with pain at the injection site (13%, 73/550 participants) the most commonly reported symptom. Only one serious adverse reaction—a case of pneumonia—was reported in the control group; however, this was unrelated to the COVID-19 vaccination.
In phase 1, 100% of participants in both the 1.5μg and 3μg groups (27/27 and 26/26 participants, respectively) generated antibodies against SARS-CoV-2. Stronger immune responses—determined by the amount of antibodies produced that can neutralise the virus, expressed as geometric mean titre (GMT) – were detected among the 3μg group compared with the 1.5μg group (GMTs of 117 and 55, respectively). In phase 2, 97% (180/186) of participants in the 1.5μg group produced antibodies against SARS-CoV-2, compared with 100% (180/180 participants) in the 3μg group. Participants in the 3μg group again produced a stronger immune response that those in the 1.5μg group (GMTs of 142 and 86, respectively). Similar to findings for other vaccines that increasing age is linked with reduced immune responses, the authors note that immune responses among children and adolescents were higher than those in adults aged 18-59 years and elderly aged 60 years and older (GMTs of 44 and 42, respectively).
No significant differences in immune response were detected in an analysis by age group, with more than 93% of those in the 1.5μg and 3μg groups aged 3-5 years, 6-11 years, and 12-17 years producing antibodies against SARS-CoV-2 (with GMTs ranging from 78 to 146) at day 28 after the second dose. In each age group, there were significant differences in GMTs between the 1·5 μg and3·0 μg groups after the second dose, except in the group aged 12-17 years old in phase 1.
Based on their results, the authors recommend two 3μg doses of the vaccine for children and adolescents aged 3-17 years.
The authors acknowledge some limitations to their study. T cell responses—which play an important role in SARS-CoV-2 infections—were not assessed in the study, though these have been investigated in related studies. The study involved a small number of participants and all were of Han ethnicity, highlighting a need for larger studies in other regions and involving multi-ethnic populations. Long-term safety and immune response data were not available, though participants will be followed for at least 1 year. Owing to the small number of participants in the study, the results should be interpreted with caution as it was not possible to draw strong statistical conclusions.
Writing in a linked Comment, Professor Bin Cao, of the China-Japan Friendship Hospital, China, highlights the need to include children in immunisation campaigns, explaining: “Herd immunity against COVID-19 is the prerequisite to end this pandemic, either through vaccinations or natural infection. Most estimates placed the threshold at 65-70% of the population gaining immunity, mainly by vaccination. However, widely circulating virus variants and persistent hesitancy on vaccine make this threshold difficult to reach. (…) Thus, the calculation has to be revised upward and children must be covered in the immunisation campaign.”
Source: Read Full Article


