Blue Whales and Broken Hearts: A Zoologist’s Take on the Heart
Zoologist Bill Schutt’s latest book, Pump: A Natural History of the Heart, uses the anatomy of hearts and the origins of circulation to explore science and medicine. Medscape interviewed the emeritus professor of biology at LIU Post in Brookville, New York, and research associate at the American Museum of Natural History in New York City.
This interview has been edited for length and clarity.
Medscape: The book opens with the blue whale heart. Was it the most interesting one you wrote about?
Bill Schutt: It’s right up there. It was surprising for reasons that the folks at the Royal Ontario Museum, who recovered the heart, had no clue about. Of course it was large, but it was a lot smaller than they thought it was going to be. I thought it was an intriguing way to open the book.
It started out tragically with nine blue whales running aground in Newfoundland (a decent percentage of the Canadian blue whale population). Not a lot was known about these creatures because they usually sink when they die. The museum folks think they came ashore because they were propped up on the ice flow, so they rushed up with construction equipment and they were able to salvage this heart.
The shape of it was surprising. I described it in the book as looking like a 400-lb soup dumpling. It didn’t look like a heart you would get from the butcher — those hearts have form and a firm structure. This was bifurcated at the bottom and it collapsed in a heap when they removed it. Even after 5 years of preservation efforts, there are still blood vessels on it that they don’t quite understand.
You write that the heart collapsing may allow whales to dive deep, right?
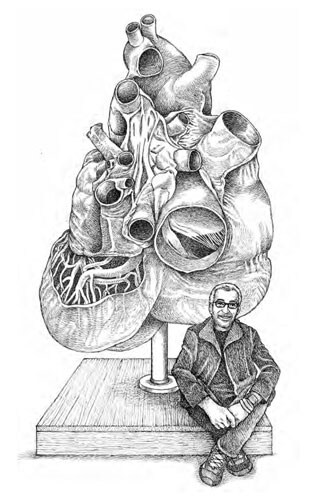
An illustration of Schutt with the plastinated blue whale heart
Yes. If you were to look at the muscle fibers on a human heart they sort of wind around the heart. When our heart beats, it’s almost like you wring it out. But in the blue whale heart, the muscle fibers run up and down. And so when they pulled this thing out, it collapsed.
They now think that this may be an adaptation to deep dives, where the pressure is so great that, rather than withstanding this tremendous pressure from a dive of thousands of feet, the heart collapses. It’s only beating two or three times per minute, so there’s no requirement for a big, sturdy structure that’s actively pumping blood. That was a real surprise to them.
While smaller than expected, is it still the biggest animal heart?
We think the blue whale heart is the biggest in the world. They used to think it was the size of a sedan, but in reality it’s more like the size of a golf cart.
The museum just got a new heart from another large whale species, so they’re excited because one of the coolest ways to do research in anatomy is to compare an organ or structure in a closely related species.
They had the blue whale heart plastinated in Germany. If you’ve seen the “Body Worlds” exhibit, it was done by that plastinarium in Germany. It was the largest structure that they’d ever plastinated, and it’s on display at the Royal Ontario Museum in Toronto (in a new exhibition on whales through March).
Is it true that in relative terms, the hummingbird may have a “bigger” heart?
If the museum had a 90-ton hummingbird sitting next to blue whale, it’s heart would be eight times larger.
The hummingbird’s wings beat 80 times per second and to supply those wing muscles with blood, oxygen, and nutrients, the heart beats 1260 times per minute. If you think of the heart as a machine, that’s probably about the upper limit.
The only other way to get enough blood to those wing muscles would be to have a larger heart, so that each time it pumps it sends more blood out.
If you’re looking at percentage of body size, the heart is about .03% of the blue whale’s body mass; for the hummingbird, it’s about 2.4% — roughly eight times larger in proportion to its body.
Can you review for our readers the section on how Galen (or belief in his theories) held medicine back?
I was interested in where the idea come from that the heart is the center of the soul and emotion. I was going to name that chapter “Blame it on the ancient Egyptians.” They thought the heart was extremely important and they didn’t really care much for the brain. When they mummified you, they would yank your brain out of your nose with a hook, but they preserved and took great care of the heart, because they thought it really was the seed of what we would call the soul.
It’s tough to decipher some of the papyrus writings, but the Egyptians characterized heart attacks and aneurysms, but they also got a lot wrong. For example, they thought that the arteries carried air. The Egyptian writings were held in high esteem by the Greeks, and we’re talking about some heavy hitters, Aristotle and Hippocrates. They picked up on the idea that the heart was the center of emotion and was vastly important; the brain was thought of as a radiator to cool the heart.
That got passed to the Romans, and within the Romans, Galen was a surgeon in the second century CE. He was hamstrung by the fact that they were not allowed to perform dissections on humans. This was a carryover from the ancient Greeks who did not allow human dissections, because the corpses were considered impure.
Galen was reduced to using animals to make statements about human anatomy and physiology, and he got a lot wrong. He believed that there were two separate circulatory systems: air mixed with this spiritual material from the atmosphere in one side, and then the venous side connected to the liver with blood being produced by the liver. Galen and his followers probably wrote 3 million words. When Rome fell, his work was not immediately translated into Latin (Latin was the language of scholarship in the West).
We believe Galen was a monotheist, but we don’t think he was a Christian. In the early Middle Ages, his work was translated into Arabic by Syrian Christians and they gave it a Christian slant. And so when that Arabic version was finally translated into Latin, the church fell in love with it because it had a Christian root. Galen’s word, which was wrong to begin with, was then probably mistranslated and was determined to be divinely inspired. You were not allowed to question it or experiment on humans, and it stayed that way for 1500 years. So while there were innovations in other areas from architecture, the arts, and more, medicine pretty much stood still, because of this adherence to Galen.
That’s not to say that, elsewhere, they weren’t making strides with regard to medicine; it just didn’t get the airplay in the West.
Is the adherence to Galen partly responsible for the obsession with bleeding and leeches?
Absolutely. Galen was into bleeding — the idea that if you were feverish and looked flushed, you had too much blood, so they would drain it. I tell the story of George Washington, who died in 1799. He had a throat infection, and over the course of a day, his physicians bled him so he lost roughly 40% of his blood. He probably died of hemorrhagic shock, combined with this throat infection.
I went to the original writings about the hearing that took place after he passed away because he was arguably the most famous person in the world at the time. I thought, ‘Here’s where I get to see how these guys screwed up,’ but the descriptions of how the physicians messed up was that they should have bled him closer to his throat, that they should have wrapped his feet in bags of salt, and they should have given him another enema.
They didn’t ‘mess up’ by bleeding him — this was recommended medical practice for years. Even if it were 1899, everything would likely have been the same, except they would have used leeches on Washington.
Can you tell us about the misperception that William Harvey discovered circulation?
No one knew how to track the blood from the body to the lungs, or from the heart to the lungs, and then back to the heart again — they got that wrong for a long, long time. Largely because Galen thought that there were two sides. Blood was on the right side, but he believed some of the blood moved over to the left side via invisible perforations in the intraventricular wall.
That belief sat around for 1500 years, but there were physicians, like Ibn al-Nafis, a 13th century Syrian who got it right. If you look at his writings, he accurately describes (what Galen never realized) that a tremendous amount of blood was coming from the lungs and going to the left side of the heart, so you didn’t need the ‘perforations.’
Several Europeans got it right 50-75 years before. Dr William Harvey was the one who publicized it in 1628. He’s the one who really clarified the idea of how the blood moves from the heart to the lungs then back to the heart and then out to the body. He got the airplay, not so much the other guys. They were up against the Galen and they were in places where no one was reading their work.
Ibn al-Nafis’ work was rediscovered in the 1920s. They found a copy of his book in a Berlin library. He got there first, but if you’re on Jeopardy and the clue is, ‘He discovered pulmonary circulation,’ then the answer is probably William Harvey. It’d be interesting to see if you get it wrong if you answered, Ibn al-Nafis.
Before writing the book, you were concerned that you wouldn’t find any interesting stories about the heart, but the origin of cardiac catheterization is pretty interesting?
I also write novels, and if you had asked me to come up with a crazy story about the first cardiac catheterization, I could not have dreamt up anything quite as bizarre as Werner Forssmann.
He was a resident at a hospital in Berlin in 1928. At the time, the way to get anything directly into the heart was to inject it in, which was problematic because you could puncture a coronary artery trying to put a hypodermic needle into a moving heart. The only other way would be to open up the chest.
Forssmann had seen photographic prints where they inserted a catheter into the jugular vein of a horse, and they put this catheter into the right atrium to measure the pressure. He thought, ‘Well why can’t we do that?’ He suggested that there was a direct route from the antecubital vein (in the bend of your elbow) that went directly into the right atrium. The hospital told him no.
He convinced a nurse to help and they snuck into the hospital one night. He had convinced her to be the subject, but in reality, the only reason he asked her was because she had the key to the cabinet where the urinary catheters were. He strapped her down on a gurney and walked away. When he came back, he already had the catheter in himself. He had moved it up about a foot toward his heart. After a bit of an argument, he untied the nurse and they went to the X-ray room to take a picture. He first had to fight off this guy who tried to pull the catheter out. They take the pictures and he’s short, the catheter is not quite into the atrium, so he pushes it in a little further and he can see this in real time on the fluoroscope. Finally, he gets it in and now he’s got the photographic evidence.
His supervisors were not thrilled. They thought he was doing it to become famous (I don’t believe he was) and he got the boot from the hospital. To make a wild story shorter, he got thrown out of a couple of different places because he’s always trying to experiment on himself. In fact the title of his memoir was, “Experiments on Myself.” He wound up becoming an army physician for the Germans during World War II. He was captured and thrown in jail as a POW. He had joined the Nazi Party in 1932 — if you asked him it was because he didn’t like the communists.
He was not able to practice medicine for several years and became a lumberjack. His wife was a general practitioner and she had access to urinary catheters so he could keep experimenting on himself. Years later, he saw that the technique that he had developed had become incredibly important. He died in 1979, but we now use cardiac catheterization, for installing valves, delivering medicine to specific regions of the brain, making specific measurements of pressure, etc. He eventually was awarded the 1956 Nobel Prize in Physiology or Medicine [along with two others], but, yeah, there’s no chance I could have dreamt that one up.
You also wrote about organ transplants. What do you think of the recent news about the attachment of a pig kidney to a human?
For the pig organ, they’re using CRISPR gene splicing technology to overcome some of the problems that would occur if you were to transplant a pig heart into a human. There are specific sugars that pigs produce that our body would have an immune reaction to and reject that organ.
They’re snipping out the part of the pig’s genetic blueprint (DNA) that produces those sugars, so you breed pigs that don’t produce the substance that a human would have a reaction to. Theoretically, you could also breed strains of pigs that are not susceptible to porcine viruses that might be transmitted to humans. That’s one way that they’re doing xenotransplants — transplants from other species to humans.
When I was writing “Pump,” I got to talk to researchers who are taking another route.
Do you mean the work of Harald Ott’s team at Harvard?
Yes. They’re taking cadaver hearts and putting them through a kind of detergent drip that drips through the heart over days and removes all of the cells that your body would possibly reject if a transplant took place. All of the muscle tissue, for example, is dissolved away. You’re left with a ghostly white heart made of connective tissue; a lot of it is collagen.
The idea is to then take common cells, fibroblasts, from the person who is going to be the recipient of this heart. You then stimulate those cells to become stem cells and the body can stimulate stem cells to become any type of cell. The technology exists to create cardiac muscle cells that can be cultured, that are specific for that recipient. Now they take those cells and embed them onto this model and, in a sense, build a heart that is specific for that recipient.
I was blown away by this and I asked Ott how long until you’re doing this on humans. He said within 10 years. That, to me, was amazing.
Presumably, if this works it could be applied to other organs.
Yes. We just don’t have enough donor organs. There are thousands of people who die every year waiting for, not just hearts, but kidneys and livers with the correct tissue type and the correct blood type.
Were any researchers reluctant to let a zoologist come and look at what they’re doing?
I started at the American Museum of Natural History as a grad student at Cornell. I have an academic background and have written a lot of scientific papers so I did my chores back in the day.
For the various books I’ve written, I’ve probably interviewed 60 or 70 experts in all sorts of fields, and I’d say 98% of them have been really quick to respond to my requests. My cover letter explains my connections and my background. I’m able to get them to talk about things that they might not talk about to the press, because they often get burned by the media.
You started out curious about how the heart became known as the center of emotion. What do you now think about heart-emotion connection, because there does seem to be some link with conditions like takotsubo syndrome?
I spent all this time going over the fact that the Egyptians, the Greeks, and the Romans had got it wrong and that there really is no connection between the heart and the mind — but in reality there is. It’s just very different than what we’ve thought for the last 2000 years.
The example that I give is takotsubo syndrome. In 1990, researchers in Japan published a paper on 30 patients, most of them postmenopausal women, who showed up at hospitals exhibiting symptoms of a heart attack — chest pain and shortness of breath. And when they did the workup on these folks they didn’t find any blockages in the coronary arteries. But when they did a ventricular gram, the left ventricle looked really strange: it was rounded at the bottom and narrow at the top, and it reminded them of the traps that their octopus fishermen use called takotsubo.
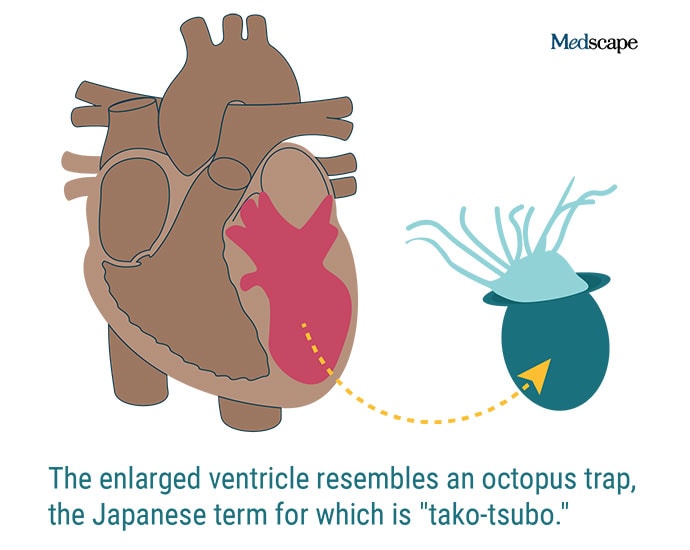
They found that all of the women had had some type of traumatic emotional experience relatively recently — they’d lost loved ones, or a job, or a house, etc etc. The researchers hypothesized that emotional trauma triggers the ‘fight or flight’ portion of your autonomic nervous system to kick in and release stress hormones into the circulatory system. This raises your blood pressure, your heart rate, your respiratory rate, dilates your pupils so that you can deal with the threat — whether real or imagined.
Now, when that threat goes away or that emotional crisis ends, the system downregulates and you come out the other side. In takotsubo, or what we often call broken heart syndrome, they think that there’s a hyperrelease of stress hormones that is not downregulated after the traumatic emotional event.
They think this causes the coronary arteries to spasm and close, cutting off flow to different parts of the heart, which stimulates pain receptors to say you’re having a heart attack. Longer-term chronic stress could irritate the heart and cause inflammation of the lining of the blood vessels. The good news is that they found the vast majority of these patients recovered within 3-6 months.
So there is this connection between the heart and the mind. It’s just very different than what we historically thought it was.
Where can readers interested in following your work find you?
“Pump” is available wherever you buy books. I have a website https://billschutt.com/ and I’m on Twitter @BillSchuttBooks, Facebook, goodreads, Amazon, the whole nine yards. I’m always happy to hear from folks.
Tricia Ward is an executive editor at Medscape. She has written about science and medicine for both consumer and healthcare professional audiences for various publications. Follow her on Twitter @_triciaward.
Follow theheart.org | Medscape Cardiology on Twitter
Source: Read Full Article


