Herd immunity is a dangerous strategy for fighting COVID-19, says expert
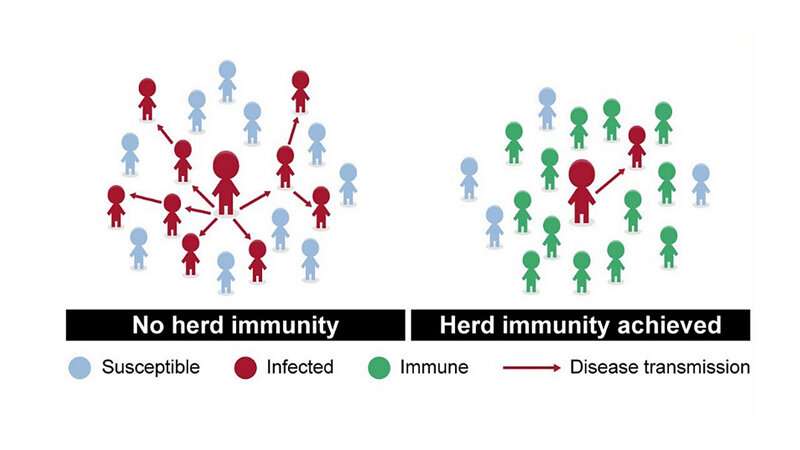
Herd immunity—when the prevalence of immunity to a virus in a population reaches “herd” levels (enough people are resistant to keep an epidemic from growing)—has been considered by some countries as a strategy to combat the current COVID-19 crisis. However, according to Stuart Ray, M.D., professor of medicine at the Johns Hopkins University School of Medicine, rushing toward herd immunity by ignoring risky behavior in the hope that infected people will survive, become resistant and reduce the susceptible population is an approach that will increase deaths and disability, and should be avoided.
“For a highly infectious virus like SARS-CoV-2 [the virus that causes COVID-19], the minimal level to reach herd immunity—where we’d expect newly infected people to pass the virus to less than one additional person—is thought to be about 60% of the population,” says Ray, noting that estimates of that level vary. “Even if testing positive for antibodies to the virus indicates that immunity gained will be more than temporary, we are probably far from that threshold.”
“In fact, in countries that have avoided lockdowns, masks and physical distancing, we have not seen evidence that any have achieved herd protection on a national scale,” he adds.
Take for example, Sweden, a major country that prominently tried herd immunity earlier this year as a national strategy. As part of the plan, Swedish officials allowed the following to remain operating without restrictions: restaurants, preschools and grade schools, public transportation, public parks, hair salons, yoga studios, gyms, malls, movie theaters and ski slopes. They did limit public gatherings to 50 or fewer people, closed high schools and universities, closed museums, cancelled public sporting events and banned visits to nursing homes. Social distancing, however, was voluntary.
The results of Sweden’s decision to attempt herd immunity were disappointing—and devastating. By the end of May 2020, the nation recorded nearly 41,000 COVID-19 cases resulting in more than 4,500 deaths in a population of 10 million, compared with Scandinavian neighbors Norway and Finland that counted fewer than 600 COVID-19 deaths combined. Anders Tegnell, Sweden’s state epidemiologist and architect of the herd immunity plan, admitted at a press conference in early June that “too many people had died too soon” as a consequence.
As for whether herd immunity could work as a strategy for the United States, the answer from Ray is an emphatic “no.” That is unless, he says, much more effective treatments are developed.
“The United States has a large vulnerable population; differing strategies at community, state and national levels for dealing with COVID-19; and a health care system with shortcomings and inequities, so it would be very difficult to reach the necessary level of immunity without an effective vaccine,” he says. “For example, the inconsistency in accessing COVID-19 testing in this country erodes safety and weakens confidence in what the results tell us. If you don’t know who’s infected, you can’t protect vulnerable people or determine who actually has immunity.”
Ray says the bigger question still needing an answer is whether SARS-CoV-2 infection yields long-term immunity.
“For herd immunity to work, prior exposure to SARS-CoV-2 has to prime the immune system to produce a strong response to all future contact with the virus, and in turn, make the person less infectious,” Ray explains. “We don’t know if that happens with this specific coronavirus.”
Source: Read Full Article


